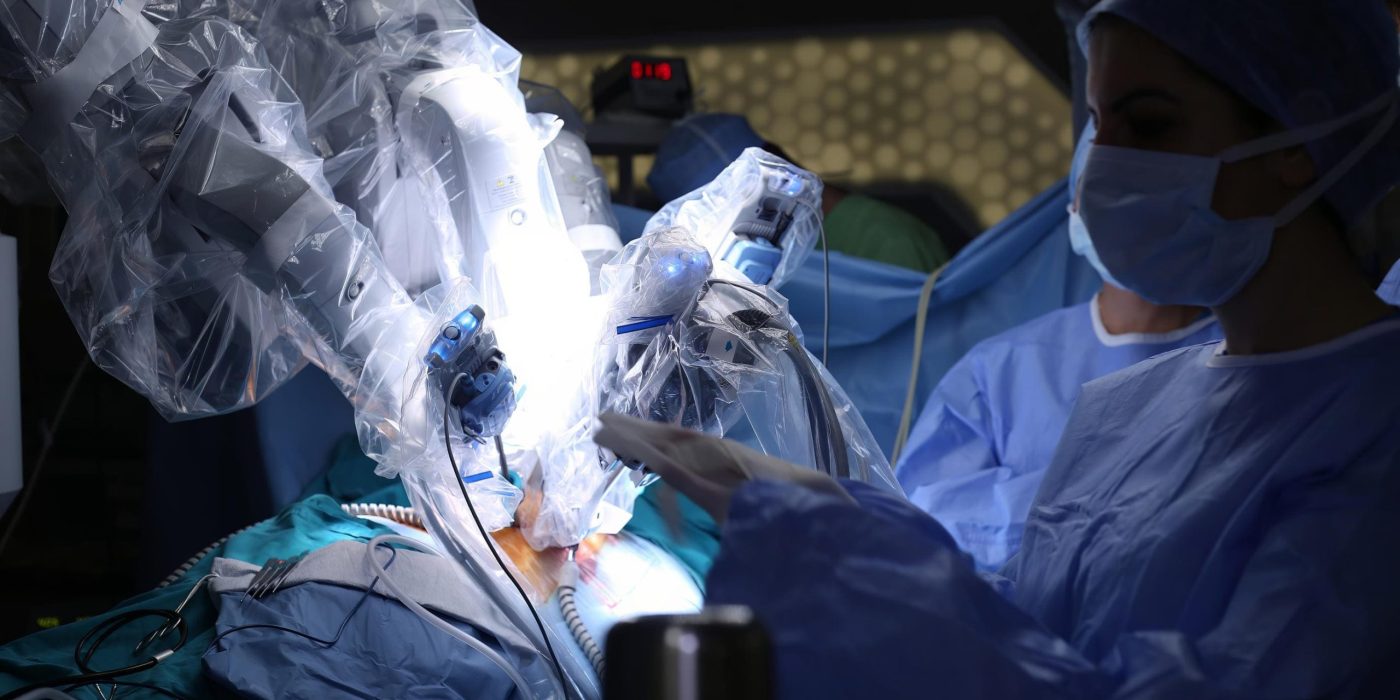
Robotic Surgery
By Dr. Markos Karavitakis, Specialized Surgeon in Laparoscopic and Robotic Surgery, Vice President of the European Association of Urology (EAU) and Director of the Center for Advanced Laparoscopic, Robotic and Endoscopic Urology Surgery Central Urology.
The history of robotic surgery
The history of robotic surgery has been a thrilling journey that redefined the approach to surgical procedures.
The year 1985, the PUMA 560, a robotic system designed for precise tasks, marked an early venture of robotic technology into surgical practices. Its success paved the way for advancements in robotics, yet it wasn't until the late 1990s that robotic-assisted surgery began gaining significant traction.
In 1997, the Robodoc system approved by FDA for orthopedic surgery, representing a milestone in the fusion of robotics with surgery. Despite facing challenges due to its complexity, limiting widespread adoption, it signaled progress in the field.
The year 2000 was a turning point with the debut of the da Vinci surgical system. Its FDA clearance for laparoscopic procedures transformed the surgical landscape, offering enhanced dexterity, magnified visualization, and a minimally invasive approach.
This caught the attention of medical professionals, culminating in the first robotically assisted heart surgery in 2002.
By 2003, the da Vinci system was utilized for various procedures, from prostatectomies to complex heart surgeries. The advancement of technology has since continued, with refined surgical techniques and the introduction of new robotic systems across different medical specialties.
The global adoption of robotic surgery has expanded, particularly led by Europe, Asia, and North America. The development of modular robotic platforms like the da Vinci Xi has brought increased flexibility and precision to surgical procedures in diverse medical fields. The widespread application of robotic technology in treating conditions such as colon cancer, kidney cancer, and obesity has underscored its promising potential.
Throughout its historical journey, robotic surgery has encountered obstacles such as cost implications, training prerequisites, and the crucial aspect of ensuring patient safety. Nevertheless, the advantages of minimized scarring, faster recovery periods, and enhanced patient outcomes have continuously fueled its progression and acceptance.
Looking forward, the history of robotic surgery paves the way for an era marked by ongoing advancements. The fusion of artificial intelligence, machine learning, and enhanced connectivity has the potential to redefine surgical accuracy, remote collaborations, and knowledge exchange among healthcare professionals. With the increasing accessibility and sophistication of this technology, the narrative of robotic surgery is poised to significantly influence the future landscape of healthcare.
Introduction of Robotic Surgery in Urology
Robotic-assisted laparoscopic surgery emerged as a viable solution to the constraints of traditional open surgery and the challenges associated with laparoscopic techniques. Since its introduction, this innovation has transformed the field of urological procedures, presenting patients with minimally invasive alternatives and empowering surgeons with unparalleled precision, control, particularly benefiting less experienced laparoscopic practitioners.
The inception of robotic surgery in the urology domain took root with the introduction of the da Vinci Surgical System in the early 2000s. This system's capacity for 3D imaging, robotic arm-facilitated enhanced dexterity, and improved ergonomic design for surgeons ushered in a new era in performing radical prostatectomies. The milestone of the first robotic-assisted laparoscopic prostatectomy in 2001 underscored the potential of this technology in urological interventions.
Over time, the utilization of robotic systems for prostatectomies has seen a substantial upsurge. A study featured in the Journal of Urology in 2018 revealed that over 80% of radical prostatectomies in the United States leveraged robotic techniques. This progressive trend reverberates globally, indicating a similar paradigm shift in urological practices worldwide
The rise of robotic surgery in urology can be largely attributed to its ability to enhance surgical outcomes. The precision and enhanced imaging provided by robotic systems contribute to decreased blood loss, shorter hospital stays, and quicker recovery times. A study in the journal European Urology from 2017 compared open and robotic-assisted radical cystectomies and revealed a notably lower complication rate and shorter hospital stay for patients who underwent robotic surgery.
Robotic surgery in urology has advanced significantly beyond prostatectomies and is now utilized in various urological procedures like nephrectomies, partial nephrectomies, pyeloplasties, and more. This progress has been supported by the introduction of new robotic platforms, like dual console systems that enable surgeons to collaborate during procedures, fostering knowledge sharing and the refinement of surgical skills.

Urological procedures performed robotically
The integration of robotic technology into urological procedures marks the dawn of a new era characterized by precise surgeries, patient-focused care, and enhanced outcomes. The proven benefits of robotic surgery in urology highlight its transformative influence on patient recovery, functional results, and overall quality of life.
- Minimally Invasive Approach: Data from numerous studies underscores the minimally invasive nature of robotic urological procedures. A 2019 study published in the journal European Urology demonstrated that robotically assisted laparoscopic prostatectomies led to significantly reduced blood loss, lower rates of wound infections, and a quicker return to normal activities compared to open surgery. The findings highlight the less invasive approach of robotic techniques, resulting in decreased post-operative pain and discomfort for patients.
- Enhanced Surgical Precision: The precision of robotic hands provides unmatched accuracy during surgery. A 2020 study published in JAMA Surgery revealed that robotic-assisted partial nephrectomies had lower rates of positive surgical margins compared to open procedures, indicating enhanced precision in tumor resection. This precision reduces the chances of disease recurrence and the need for additional interventions.
- Faster Recovery and Shorter Hospital Stays: Data on robotic urological procedures consistently showcase shorter hospital stays and faster recovery times. A 2018 study in the Journal of Urology found that patients undergoing robotic pyeloplasties had significantly shorter hospital stays and returned to full activity sooner when compared to open procedures. The data highlight the potential of robotic surgery to expedite patient recovery.
- Functional Outcomes: Preservation of functional outcomes is a key feature of robotic urological procedures. A 2019 study in the Journal of Endourology noted that patients who underwent robotic-assisted radical cystectomies had better urinary incontinence outcomes than those undergoing open procedures. These findings reinforce the benefits of robotic techniques in maintaining the quality of life of patients.
- Reduced Complication Rates: Data published in the 2021 issue of the Journal of Urology demonstrated that patients undergoing robotic-assisted radical cystectomies had markedly lower rates of intraoperative complications compared to open procedures. Studies have also exhibited reduced rates of surgical wound infections and various other complications associated with robotic methods, further highlighting the advantages of this technology.
Accumulating data emphasize the substantial advantages of robotic surgery in urology. Consistent trends such as reduced blood loss, decreased post-operative pain, shorter hospital stays, enhanced surgical precision, and improved functional outcomes characterize various robotic urological interventions. As technology advances, the integration of robotic systems with AI-based insights and enhanced visualization holds the potential to further amplify these advantages, shaping the future of urology care.
In conclusion, the evidence-based benefits of robotic surgery in urology have reshaped the landscape of patient care. The synergy between surgical expertise and robotic precision offers patients improved outcomes, faster recovery and improved quality of life. As the field advances, data-driven evidence reinforces the imperative to leverage robotic technology to redefine surgical paradigms and ultimately deliver exceptional care to urological patients worldwide.

The advantages of robotic surgery in urological procedures
The integration of robotic technology into urological procedures has introduced a new phase of surgical precision and enhanced results. The evidence-based benefits of robotic surgery in urology emphasize its influence on patient recovery, functional outcomes, and overall quality of life.
- Minimally Invasive Approach:Numerous studies emphasize the minimally invasive nature of robotic urological procedures. An article published in the 2019 issue of European Urology showcased that robotically assisted laparoscopic prostatectomies led to significantly reduced blood loss, lower rates of surgical wound infections, and quicker return to normal activities compared to the open method. These findings underscore the less invasive quality of robotic techniques, resulting in decreased post-operative pain and discomfort for patients.
- Enhanced Surgical Precision: The precision offered by robotic arms during surgery is unparalleled. Research published in JAMA Surgery in 2020 revealed that robotic-assisted partial nephrectomies exhibited lower rates of positive surgical margins compared to open procedures, indicating improved accuracy in tumor resection. This heightened accuracy diminishes the chances of disease recurrence and the necessity for additional interventions.
- Faster Recovery and Shorter Hospital Stays: The realm of robotic urology procedures is characterized by shortened hospital stays and expedited recovery times. A study in the 2018 issue of the Journal of Urology disclosed that patients undergoing robotic pyeloplasties had notably shorter hospital stays and returned to full activity faster than those undergoing open procedures. These findings underscore the potential of robotic surgery to accelerate patient recovery.
- Functional Outcomes: Preservation of functional outcomes is a key feature of robotic urological procedures. A 2019 study in the Journal of Endourology noted that patients who underwent robotic-assisted radical cystectomies had better urinary incontinence outcomes than those undergoing open procedures. These findings reinforce the benefits of robotic techniques in maintaining the quality of life of patients.
- Reduced Complication Rates: Data published in the 2021 issue of the Journal of Urology demonstrated that patients undergoing robotic-assisted radical cystectomies had markedly lower rates of intraoperative complications compared to open procedures. Studies have also exhibited reduced rates of surgical wound infections and various other complications associated with robotic methods, further highlighting the advantages of this technology.
The study data underscore the significant advantages of robotic surgery in urology, including reduced blood loss, minimized post-operative pain, shorter hospital stay, enhanced surgical precision, and improved functional outcomes across various robotic urological interventions.

Benefits of Robotic Systems in Surgery for Surgeons
The application of robotic systems in surgery offers a number of advantages for the surgeon such as:
- Enhanced Precision: Robotic systems offer unparalleled precision and control to surgeons. The robotic arms can execute intricate movements with high accuracy, facilitating precise surgical maneuvers and reducing the risk of human error.
- Improved Vision: Robotic systems provide high-definition 3D imaging, granting surgeons a detailed view of the surgical field. This enhanced vision aids in identifying anatomical structures and performing complex procedures with exceptional precision.
- Reduced Fatigue: Robotic surgery minimizes the physical strain on surgeons by providing ergonomic console designs that allow for comfortable seating and effortless operation. This setup helps in reducing fatigue during prolonged surgical procedures.
- Stability of Movements: Robotic arms can stabilize hand tremors, ensuring steady and controlled movements during surgery. This stability is particularly advantageous in procedures where precise movement is crucial.
- Remote Surgery: Advanced robotic systems enable remote surgical procedures, enabling surgeons to operate on patients from a different location. This capability has the potential to offer specialized medical care in underserved regions and emergency scenarios.
- Adaptable Movements: Robotic systems accurately replicate the movements of a surgeon's hands, providing a high degree of control over the robotic arms. Surgeons can perform intricate and customizable movements with precision and flexibility.
- Training and Skill Development: Robotic surgery serves as a valuable platform for surgeons to enhance their skills in a controlled and safe environment. The system offers simulation and training features that allow surgeons to practice various procedures before performing them on actual patients.
- Data and Analytics: Robotic systems can gather data during surgeries, offering valuable insights for post-operative analysis. This data can be utilized to refine surgical techniques, enhance patient outcomes, and optimize robotic procedures over time.

Contraindications and limitations of robotic surgery
When considering robotic surgery, it is crucial to be aware of the following contraindications. Some common contraindications include:
- Serious comorbidities: Patients with serious comorbidities like severe heart or lung disease may not be suitable candidates for this method due to increased surgical risks.
- Inaccessible Surgical Field: In cases where the surgical field is inaccessible for robotic tools, an alternative surgical approach might be necessary.
- Difficult cases from surgeons with limited experience: Surgeons with limited experience in robotic procedures may face challenges performing complex surgeries, potentially impacting the outcomes.
- Hemodynamic instability: Hemodynamically unstable patients with fluctuating blood pressure or heart rate may not be suitable for robotic surgery due to the gas insufflation requirement.
- Active infection: Active infection in the surgical area can heighten complications in robotic surgery and other procedures.
- Pregnancy: Robotic surgery is not recommended for pregnant women due to possible risks to both the patient and fetus.
- Economic issues: Financial considerations should be taken into account since robotic surgery can be costly, particularly for patients lacking adequate insurance coverage or financial resources.
It is essential for patients and surgeons to thoroughly assess each case, considering the patient's overall health, medical history, and surgical complexity to determine the suitability of robotic surgery for each individual.

Complications and risks of robotic surgery
Robotic surgery provides numerous advantages. However, it is crucial to be aware of the potential side effects and risks linked with the procedure. Typical side effects and risks of robotic surgery comprise include:
- Infection: Infection risk exists with robotic surgery, including the possibility of infections at incision sites or within the surgical field.
- Bleeding: Despite efforts to minimize blood loss, bleeding can still occur during or after robotic surgery.
- Pain and discomfort: Patients may feel pain and discomfort in and around incision sites following robotic surgery, typically temporary and manageable with pain relief medication.
- Damage to adjacent organs or tissues: Accidental harm to neighboring organs or tissues may occur during robotic surgery, particularly in cases of anatomical variations.
- Thrombosis: Surgery patients have a slightly elevated risk of developing blood clots in the legs (deep vein thrombosis) or lungs (pulmonary embolism).
- Anesthesia Complications: Anesthesia presents its own risks, such as allergic reactions, adverse drug reactions, and complications linked to the respiratory and cardiovascular systems.
- Pneumothorax: Procedures involving abdominal gas placement carry a small pneumothorax risk.
- Conversion to open surgery: Unforeseen issues or technical challenges may prompt surgeons to switch from robotic to traditional open surgery in some instances.
- Intra-abdominal effusions: Like open procedures, robotic procedures carry the risk of infections and effusion accumulation.
- Limited Tactile Feedback: Robotic surgery lacks the tactile feedback present in traditional open and laparoscopic surgeries, which can result in challenges assessing tissue characteristics.
- Longer operating time: Robotic procedures may require more time than traditional open surgeries due to setup and robotic machine adjustments.
- Cost: Robotic surgery is costly due to equipment and procedure expenses.
Despite these risks, the majority of robotic procedures are completed successfully with few complications.
